Introduction to Leukocytes
Leukocytes, commonly known as white blood cells, are crucial components of the immune system. They play a vital role in defending the body against infections and foreign invaders. Understanding their function can provide insights into how our bodies maintain health and combat disease. Leukocytes are produced in the bone marrow and are present in the blood and lymphatic system. They are larger than red blood cells but are fewer in number. Despite their small population, their impact on health is immense, as they are the first responders to infection and injury.
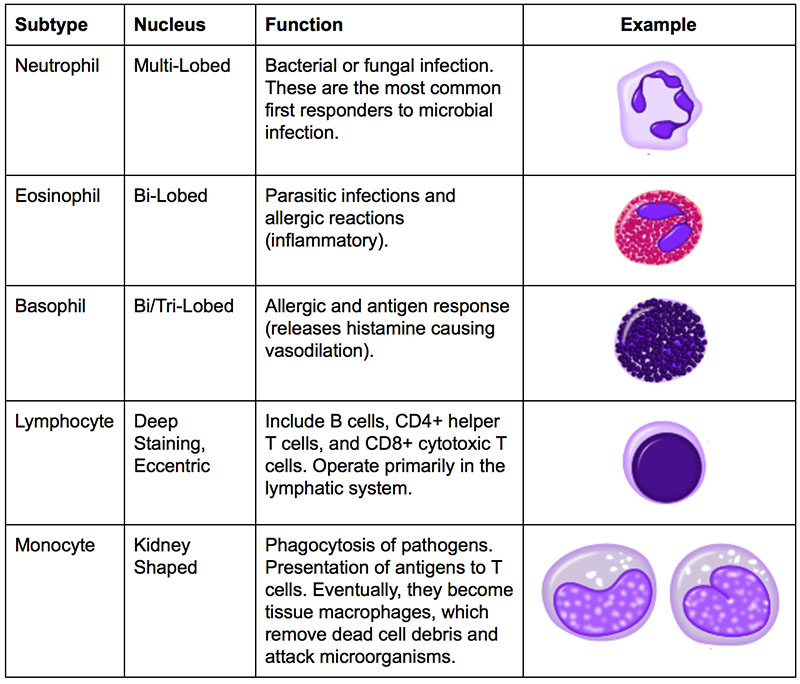
Types of Leukocytes
Leukocytes are classified into five main types: neutrophils, lymphocytes, monocytes, eosinophils, and basophils. Each type has a specific function and role in the immune response. Neutrophils are the most abundant and are the first to arrive at the site of infection. They primarily target bacteria and fungi. Lymphocytes, which include T-cells and B-cells, are central to adaptive immunity. They recognize specific pathogens and remember them for faster responses in the future. Monocytes, which develop into macrophages, are involved in phagocytosis, engulfing and digesting cellular debris and pathogens. Eosinophils and basophils are less common and are primarily involved in allergic reactions and combating parasitic infections.
The Function of Neutrophils
Neutrophils are often considered the body's first line of defense. They are highly mobile and can quickly move to sites of infection where they perform phagocytosis, engulfing and destroying pathogens. Neutrophils contain granules filled with enzymes and antimicrobial proteins that kill and digest microorganisms. They can also release extracellular traps to capture and kill pathogens. This rapid response is crucial for preventing the spread of infection. However, the activity of neutrophils is a double-edged sword; while they protect the body, their enzymes can also damage healthy tissue if not regulated properly.
Neutrophil Extracellular Traps (NETs)
Neutrophils can form neutrophil extracellular traps (NETs), which are networks of fibers composed of DNA and antimicrobial proteins. NETs trap and kill bacteria and fungi, preventing their spread. This process, known as NETosis, is a unique form of cell death distinct from apoptosis. While NETs are effective in pathogen clearance, excessive NET formation has been linked to inflammatory diseases, highlighting the need for balanced immune responses.
T-Cells and B-Cells in Adaptive Immunity
Lymphocytes, particularly T-cells and B-cells, are essential for the adaptive immune response. T-cells recognize and destroy infected cells, while B-cells produce antibodies that neutralize pathogens. T-cells mature in the thymus and are responsible for cell-mediated immunity. They include helper T-cells, which activate other immune cells, and cytotoxic T-cells, which kill infected cells. B-cells mature in the bone marrow and are responsible for humoral immunity. Upon activation, they differentiate into plasma cells that secrete antibodies. These antibodies target specific antigens, marking them for destruction by other immune cells.
Memory Cells and Immunological Memory
A unique feature of adaptive immunity is the development of immunological memory. After an infection, some T-cells and B-cells become memory cells. These cells persist in the body and respond more rapidly and effectively to subsequent exposures to the same pathogen. This principle underlies the effectiveness of vaccines, which simulate an infection to build up memory cells without causing disease. Memory cells provide long-term protection and are the reason why we often gain immunity to diseases after being exposed to them or receiving vaccinations.
The Role of Monocytes and Macrophages
Monocytes are versatile cells that circulate in the blood before migrating into tissues, where they differentiate into macrophages or dendritic cells. Macrophages are essential for phagocytosis, engulfing and digesting pathogens and dead cells. They also secrete cytokines, signaling molecules that modulate the immune response. Macrophages play a critical role in inflammation and tissue repair. They can present antigens to T-cells, linking innate and adaptive immunity. In addition to their defensive roles, macrophages help maintain tissue homeostasis by removing apoptotic cells and debris.
Eosinophils and Basophils in Allergy and Inflammation
Eosinophils and basophils are less abundant but play crucial roles in immune responses to parasitic infections and in allergic reactions. Eosinophils combat multicellular parasites and modulate allergic inflammatory responses by releasing toxic granules and cytokines. Basophils, on the other hand, release histamine and other mediators during allergic reactions, contributing to inflammation and symptom manifestation. Both cell types are involved in the regulation of inflammation and can influence the severity of allergic reactions. While they are essential for protecting against certain pathogens, their dysregulation can lead to chronic inflammatory diseases and allergies.
The Balance and Regulation of Leukocyte Activity
The immune system relies on a delicate balance of leukocyte activity to function effectively without causing damage to the body. Regulatory mechanisms ensure that leukocytes are activated only in response to genuine threats and that their actions are appropriately controlled. Dysregulation of leukocyte function can lead to autoimmune diseases, where the immune system mistakenly targets healthy cells, or immunodeficiency, where the body cannot mount an adequate response to infections. Understanding these regulatory pathways is crucial for developing therapies for immune-related diseases.
Leukocytes in Health and Disease
Leukocytes are central to maintaining health by protecting against infections and facilitating tissue repair. However, their function can be compromised in diseases such as leukemia, where there is an abnormal proliferation of white blood cells, or in conditions like HIV/AIDS, which severely deplete certain leukocyte populations. Research into leukocyte biology continues to uncover new therapeutic targets for a wide range of diseases, from cancer to autoimmune disorders. Advances in immunology have led to the development of treatments such as monoclonal antibodies and immune checkpoint inhibitors, which modulate leukocyte function to treat disease.
Conclusion: The Future of Leukocyte Research
The study of leukocytes remains a dynamic and rapidly evolving field. As our understanding of these vital cells expands, so too does our ability to manipulate them for therapeutic benefit. Future research aims to unravel the complexities of leukocyte interactions and their roles in various diseases. Personalized medicine, which tailors treatments based on individual immune profiles, represents a promising frontier in healthcare. By deepening our knowledge of leukocyte biology, we can improve diagnostics, develop novel therapies, and enhance our overall understanding of the immune system's role in health and disease.
You Might Also Like
Exploring Xbox Devices: A Comprehensive Guide For 2024Understanding Angles: Definitions, Importance, And Applications In 2024
Understanding Antibiotic Bactrim: Uses, Benefits, And Considerations In 2024
Exploring Iconic NYC: A Journey Through The Heart Of The Big Apple
Understanding Multi-Factor Authentication: A 2024 Guide To Enhanced Security
Article Recommendations
- Selena Quintanilla 90s Outfits Iconic Style Photos More
- Ryan Cameron A Pioneer In American Finance And Economic Leadership
- The Untold Story Of Bevy Smith Her Twin Sister And More